
Fighting Uneven Tone?
Hyperpigmentation impacts 1 in 3 people in the UK, primarily those over the age of 35, presenting as rough, patchy skin.
Though it does not have to be permanent. Revive sun damage, even melasma, and repair injury for real with Monderma’s powerful active ingredients.
Submit
Complete a short, free skin assessment
Start
Get your custom formula every 4 weeks
Support
Track progress, and cancel, restart anytime
What Is In Your Nightly Cream?
You will find 2-3 gold standard active ingredients, excipients, and a hyaluronic acid base cream sourced from MHRA suppliers in your hyperpigmentation fading formula.
Recyclable
Vegan Friendly
Cruelty Free
FRAGRANCE FREE
Alcohol Free
GPhC Regulated
MHRA Approved Suppliers
Dermatologist Tested
Pharmacist Led

The Monderma Difference
| Retail |  |
|---|---|
| Multiple products | All-in-one multitasker |
| Batch produced | Personalised |
| Over-the-counter | Pharmacist-led |
| Cosmetic ingredients | Active ingredients |
| Low strength | High strength |
| Rarely regulated | GPhC-regulated |
| Elementary checks | MHRA-suppliers |
| Typically imported | UK-compounded |
Transform Your Skin Today
Custom formulas are provided under the supervision of GPhC registered prescribers and pharmacists for safe, effective use.
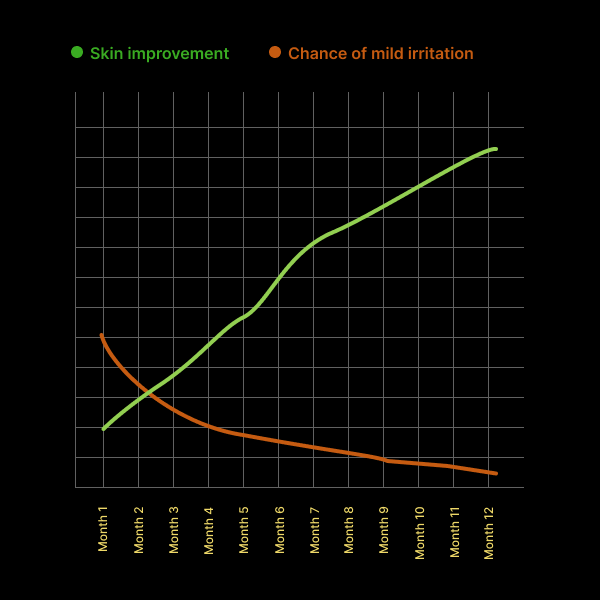
As your treatment progresses, you will notice less discolouration. Mild side effects such as peeling, tingling, and redness may occur but typically ease as your skin adjusts.
Tried, Tested, Loved: Hear It Firsthand
Changing skin without the needles!
“I was at a stage where my skin felt quite dull, tired and dry. I forged this part of my daily evening routine and my god…. Thanks for making this for me!!”
– Kavita, G, Oxfordshire, UK
Monderma is a skincare saviour
“Small areas of freckling and pigmentation have disappeared, the texture of my skin is smooth and even and my skin looks better now than 10 years ago!”
– Sarah, V, Oxfordshire, UK

Brighten your skin’s future with personalised skincare up to 20x the strength of over-the-counter depigmentation products.
Still Have Questions?
Hyperpigmentation is a chronic skin condition that affects 1 in 3 people in the UK, typically those over the age of 35.
It tends to affect women more than men.
Hyperpigmentation is more common in people with darker skin tones, but it is still significant in those with lighter skin tones.
The symptoms of hyperpigmentation are patches of skin becoming darker than the surrounding skin.
The face is the most commonly affected area, accounting for 90% of all cases of hyperpigmentation. It also affects 20% of people on the neck and chest, 10% on the shoulders and back, 30% on the arms and 10% on the legs.
Hyperpigmentation consists of 3 subtypes:
| Subtype | Description | Common Areas |
|---|---|---|
| Solar Lentigines (age, liver, or sun spots) | Flat, brown, or black spots, small and can cluster, with a smooth texture | Exposed areas of the skin, including the face, neck, arms, and legs |
| Melasma (chloasma or the mask of pregnancy) | Flat, brown or grey-brown patches, with irregular, blotchy pigmentation, and symmetrical distribution | Face, neck, stomach, and forearms |
| Post-Inflammatory Hyperpigmentation(PIH) | Flat, red, brown, or black spots or patches following inflammation or injury, varying in size | Any area of the body that has experienced inflammation due to a skin condition such as acne or eczema, or from an injury, like a cut or burn |
Around 50% of people with hyperpigmentation develop solar lentigines, 25% melasma, and 50% post-inflammatory hyperpigmentation.
The term “hyper” refers to more, whereas “pigment” denotes colour.
Hyperpigmentation is caused by an overproduction of melanin, the pigment that is responsible for the colour of the hair, eyes, and skin.
The causes of hyperpigmentation include:
| Cause | Description |
|---|---|
| Photoageing | Photoageing, caused by prolonged and unprotected exposure to ultraviolet (UV) radiation, is the leading causes of solar lentigines. While primarily resulting from sun exposure, artificial UV sources like tanning beds can contribute. Over time, cumulative UV radiation stimulates melanin production in areas most frequently exposed to the sun, such as the face, arms, and hands, leading to the formation of sun spots |
| Injury | Injury to the skin, whether from acne, eczema, burns, or wounds, causes inflammation. As the skin heals, it can produce excess melanin, which gets deposited in the injured area, resulting in dark spots or patches that can appear red, brown, grey, or black, depending on the person’s skin tone. Further irritation, like rubbing or scratching the area, can worsen this post-inflammatory hyperpigmentation. Additionally, fungal, viral, or bacterial infections may contribute to hyperpigmentation during the healing process |
Several other factors can influence the development of the condition. This includes:
| Contributor | Description |
|---|---|
| Genetics | Genetics influence the likelihood of developing hyperpigmentation, with some people naturally more predisposed. For example, freckles are often inherited and more common in people with fair skin because of the MC1R gene. Melasma tends to run in families. Lentigines are linked to genetic conditions like LEOPARD or Peutz-Jeghers syndromes. Congenital dermal melanocytosis (CDM), often seen in some ethnic groups, is genetic. People with darker skin are more genetically predisposed to post-inflammatory hyperpigmentation because their skin cells produce more pigment |
| Hormones | Hormones, particularly oestrogen and progesterone can cause an increase melanin, especially during pregnancy or from birth control, leading to conditions like melasma. Adrenocorticotropic hormone (ACTH) triggers melanin production, causing dark spots in conditions like Addison's disease. Melanocyte-stimulating hormone (MSH) boosts melanin levels and can be influenced by stress or pregnancy. Thyroid imbalances, especially hypothyroidism, and insulin resistance can lead to darker patches like acanthosis nigricans |
| Medications | Medications can increase melanin production or depositing pigments in the skin. Antibiotics, such as tetracyclines, can cause hyperpigmentation, particularly in areas exposed to the sun. Antimalarial drugs, like chloroquine and hydroxychloroquine, can lead to blue-grey pigmentation, especially on the face. Oestrogen and progesterone found in birth control pills or hormone replacement therapy can cause melasma. Nonsteroidal anti-inflammatory drugs (NSAID’s), amiodarone, used for heart conditions, and anticonvulsants like phenytoin can result in pigmentation changes as well. Chemotherapy drugs, such as bleomycin and busulfan, are known to cause dark patches on the skin |
Hyperpigmentation is common on darker skin tones, which already have a higher melanin content.
A doctor, pharmacist, or nurse can diagnose hyperpigmentation by performing a physical examination to assess the extent and severity of the affected areas, and reviewing the patient’s medical history.
Its clinical manifestations can vary widely, and diagnosis relies on recognising characteristic patterns and understanding potential contributing factors.
The severity of hyperpigmentation can range from mild, localized discoloration to extensive, darker patches.
| Severity | Distribution | Characteristics |
|---|---|---|
| Mild | 1-19% | Localised areas on sun-exposed areas |
| Moderate | 20-49% | Noticeable patches of darker skin, more frequent, and larger spots |
| Severe | >50% | Deep, dark patches, extensive uneven skin tone |
When diagnosing hyperpigmentation, it's important to consider other conditions that may present with similar symptoms:
| Condition | Description |
|---|---|
| Acanthosis Nigricans | Acanthosis Nigricans manifests as dark, thick, velvety patches in skin folds like the back of the neck, armpits, and groins, and is often associated with insulin resistance, obesity, or hormonal conditions like PCOS |
| Addison's Disease | Addison's Disease leads to generalised skin darkening, particularly on pressure points and skin folds, due to adrenal dysfunction, and is usually accompanied by fatigue and low blood pressure |
| Erythema Dyschromicum Perstans | Erythema Dyschromicum Perstans is characterised by greyish or ashy patches on the face and neck, frequently linked to genetic and environmental factors, and is more common in darker skin tones |
| Hemochromatosis | Hemochromatosis results in bronzed or darker skin due to excess iron deposits, typically accompanied by liver disease and joint pain |
| Lichen Planus Pigmentosus | Lichen Planus Pigmentosus causes dark patches on the face and neck, is often linked to autoimmune conditions or sun exposure, and is more common in darker skin tones |
| Lupus Erythematosus | Lupus Erythematosus often leads to dark spots following a red rash, especially on sun-exposed areas like the nose and cheeks, and is associated with joint pain and fatigue |
| Peutz-Jeghers Syndrome | Peutz-Jeghers Syndrome presents with dark spots around the mouth and fingers, which are frequently associated with gastrointestinal polyps and an increased cancer risk |
| Tinea Versicolor | Tinea Versicolor appears as fungal infection-induced patches of lighter or darker skin, commonly on the chest or back, affecting melanin production |
A skin biopsy may be necessary to rule out another condition.
If the skin has not responded to over-the-counter products or is at risk of complications, Monderma may recommend a treatment plan.
This may contain up to 3 of the following ingredients:
| Topical | Properties |
|---|---|
| Retinoids | Regulate the growth of cells on the skin to improve its texture and tone |
| Lightening Agents | Reduce the production of melanin to lighten patches of darker skin |
| Anti-Inflammatories | Inhibit the production of inflammatory-causing molecules to reduce redness and irritation |
| Corticosteroids | Inhibit the production of melanin to reduce swelling and inflammation |
| Antioxidants | Eliminate free radicals by repairing and strengthening the barrier function of the skin, improving hydration |
Treating ageing skin topically must include adopting daily use of broad-spectrum sunscreen of SPF30 or higher. It can take 8 weeks or longer to see lasting results, so it is important to be patient and follow your treatment plan. Information on these ingredients, their directions for use, safety information, storage, potential side effects, and reporting can be found in the information leaflet
People with hyperpigmentation that changes colour or does not improve with treatment should consult a doctor, chemist, or nurse. They will conduct a more thorough examination of the condition and, if necessary, perform a skin biopsy.
The complications and challenges associated with hyperpigmentation include:
| Complication | Description |
|---|---|
| Recurrence | In cases of post-inflammatory hyperpigmentation (PIH), ongoing skin inflammation can result in pigmentation to persist and worsen over time. Even after successful treatment, hyperpigmentation may reappear if the underlying cause is not addressed and proper sun protection practices are not followed |
| Scarring | Scarring can occur, primarily as a result of post-inflammatory hyperpigmentation. When the skin is repeatedly injured, irritated, or exposed to sunlight without protection, the risk of deeper and longer-lasting pigmentation rises, resulting in uneven skin texture and tone. In some cases, this could be more difficult to treat than the original hyperpigmentation. Acne-related hyperpigmentation may indicate deeper scarring, requiring more intensive treatment |
| Texture Changes | Texture changes in hyperpigmentation occur when the skin becomes uneven, rough, or raised as a result of inflammation or injury. These changes often accompany dark spots, particularly when the healing process is hampered by factors like picking at wounds or sun exposure. The combination of discolouration and irregular texture can make hyperpigmentation more visible |
| Treatment-Related | Treatment like microdermabrasion, chemical peels, and laser therapy carry risks such as scarring, infection, or worsened pigmentation if not performed correctly or without proper aftercare. Furthermore, if applied inconsistently or without professional guidance, both topical treatments and procedures can result in uneven skin tone, and allergic reactions to topical ingredients can aggravate the skin, exacerbating hyperpigmentation |
| Underlying Health Conditions | Underlying health conditions can be associated with a variety of pigmentation changes, most notably disruptions in melanin production. Inflammatory conditions such as acne, eczema, and psoriasis can cause post-inflammatory hyperpigmentation. Hormonal imbalances, such as those seen during pregnancy or with the use of birth control, can result in melasma. Addison's disease, a disorder of the adrenal glands, causes widespread skin darkening due to increased adrenocorticotropic hormone (ACTH). Insulin resistance in polycystic ovary syndrome (PCOS) can cause dark patches, particularly on the neck and armpits. Furthermore, certain metabolic or genetic conditions, such as hemochromatosis or Peutz-Jeghers syndrome, can cause an increase in pigmentation |
| Psychosocial | Psychosocial impacts of hyperpigmented areas, particularly those that are prominent or widespread, can lead to feelings of self-consciousness and low self-esteem. People may experience anxiety, depression, or emotional distress as a result of how their skin appears. Some people may avoid social situations, outdoor activities, or wearing clothing that reveals the affected areas, which can reduce quality of life and self-expression |
Addressing hyperpigmentation early and adhering to sun protection measures are key steps in minimising the risk of complications and improving skin appearance and overall wellbeing.




