Overview
Hyperpigmentation is classified as solar lentigines, melasma, or post-inflammatory hyperpigmentation

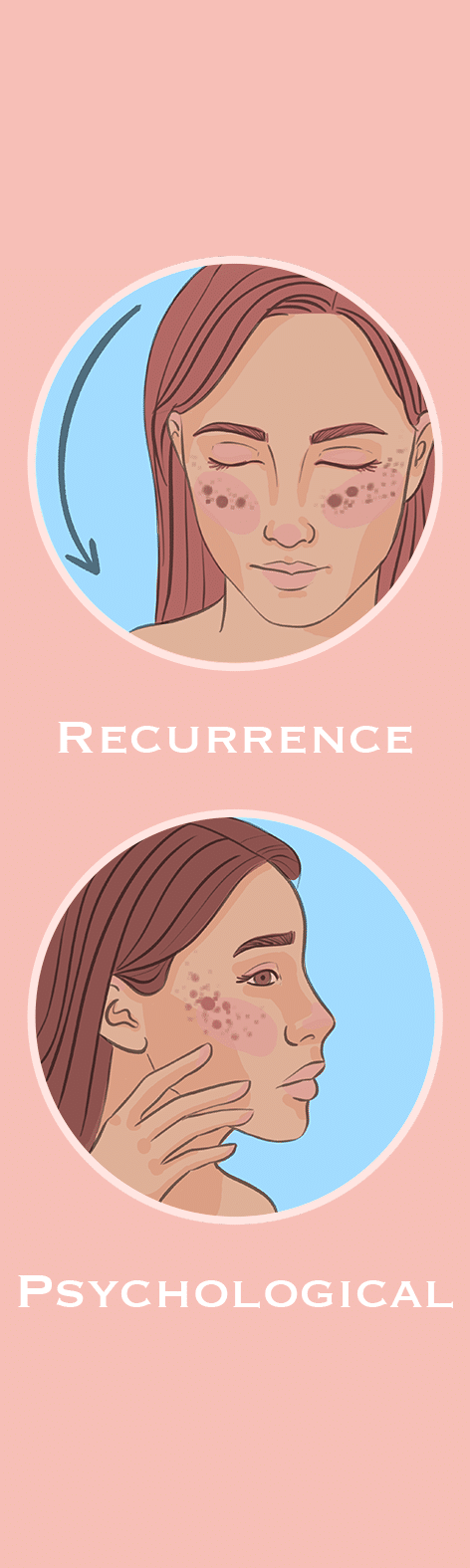
Hyperpigmentation is a chronic skin condition that affects 1 in 3 people in the UK, typically those over the age of 35.
It tends to affect women more than men.
Hyperpigmentation is more common in people with darker skin tones, but it is still significant in those with lighter skin tones.
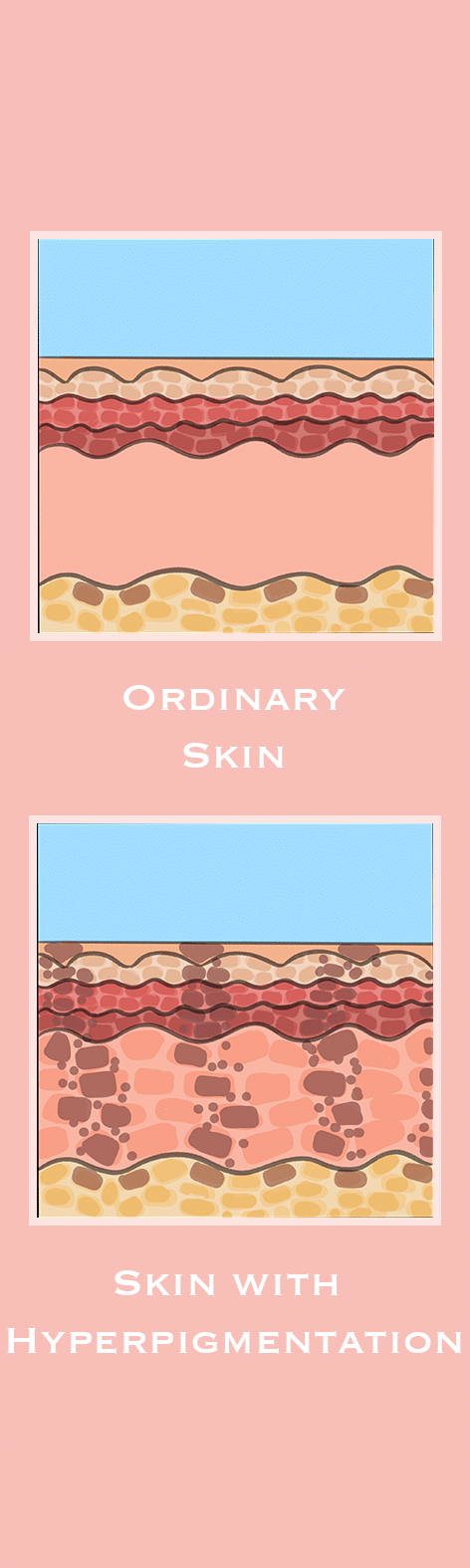
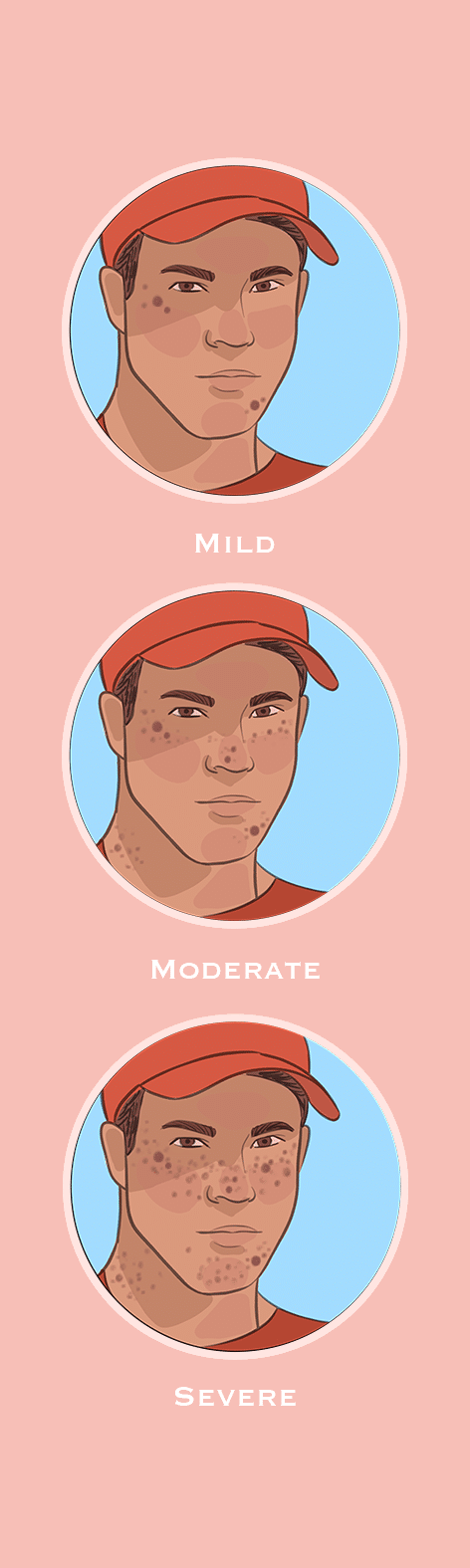
The symptoms of hyperpigmentation are patches of skin becoming darker than the surrounding skin.
The face is the most commonly affected area, accounting for 90% of all cases of hyperpigmentation. It also affects 20% of people on the neck and chest, 10% on the shoulders and back, 30% on the arms and 10% on the legs.
Hyperpigmentation consists of 3 subtypes:
| Subtype | Description | Common Areas |
| Solar Lentigines
(age, liver, or sun spots) |
Flat, brown, or black spots, small and can cluster, with a smooth texture | Exposed areas of the skin, including the face, neck, arms, and legs |
| Melasma
(chloasma or the mask of pregnancy) |
Flat, brown or grey-brown patches, with irregular, blotchy pigmentation, and symmetrical distribution | Face, neck, stomach, and forearms |
| Post-Inflammatory Hyperpigmentation
(PIH) |
Flat, red, brown, or black spots or patches following inflammation or injury, varying in size | Any area of the body that has experienced inflammation due to a skin condition such as acne or eczema, or from an injury, like a cut or burn |
Around 50% of people with hyperpigmentation develop solar lentigines, 25% melasma, and 50% post-inflammatory hyperpigmentation.
The term “hyper” refers to more, whereas “pigment” denotes colour.